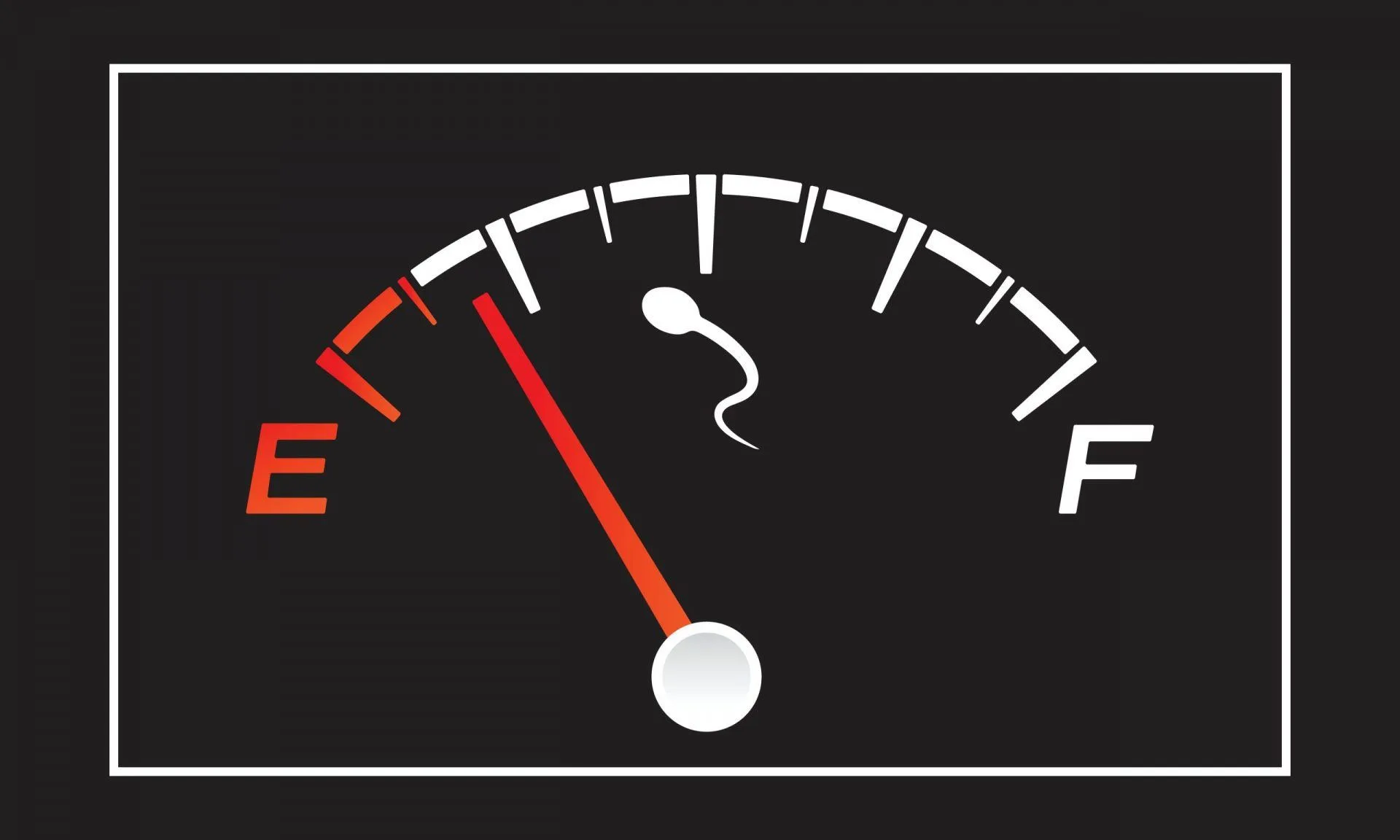
The month of November is usually focused on men’s health and longevity, with attention being paid to the various health issues that affect the male demographic. In honor of men’s health month, a recent study reported that we may be in the midst of a reproductive crisis, as researchers are warning that sperm count is declining at an accelerated rate.
What’s Happening To Men’s Sperm?
In 2017, researchers published a study in the Human Reproduction Update journal that found that sperm count had more than halved in the last 40 years. Unfortunately, the study was critiqued for only featuring North America, Europe, Australia, and New Zealand in their findings.
So, in an effort to update their findings, as well as to diversify the study, the same team of researchers evaluated 38 studies that had recorded men’s sperm counts and were published between 2014 and 2020. They combined the 38 studies with other studies that had been featured in their 2017 review, extracted the data, and fed it into models. This means that the new study included data from more than 57 000 men collected over 223 studies across 53 countries.
Is The World’s Sperm Count in Trouble?
According to the findings, published in Human Reproduction Update, the average sperm count had dropped by slightly more than 1% per year between 1973 and 2018. On a global scale, the average sperm count had fallen by 62.3% between 1973 and 2018.

kenary820/Shutterstoc
Additionally, the researchers also noted that the rate at which sperm count was declining was accelerating, going from an average of 1.16% per year after 1973 to 2.64% per year after 2020.
The sperm concentration had fallen 51.6% by 2018, with the average sperm concentration falling from an estimated 101.2 m per ml to 49.0 m per ml between 1973 and 2018.
Sperm concentration refers to to the number of sperm per milliliter of semen, whereas total sperm count is the total number of sperm in the entire ejaculate.
Granted, the sperm count number is still above the cutoff of 15 million per milliliter, which indicates a low sperm concentration. However, the drop is still alarming, and it still requires our attention.
“We have a serious problem on our hands that, if not mitigated, could threaten mankind’s survival,” – Prof. Hagai Levine of the Hebrew University of Jerusalem, co-study lead.
What causes low sperm count?
While Prof. Levine admits that the study didn’t address what may be causing the decline, previous research has indicated factors that may affect sperm count. These include:
- Obesity: One study found that obese men face a 42% increased risk of having a low sperm count and an 81% increased risk of likely producing no sperm. However, a more recent study found that obese men who lose weight can improve their sperm count by 40%.
- Sedentary living: Exercise can improve your health in a number of ways. In fact, research from Harvard Health found that men who regularly exercise for 15 or more hours weekly experienced a 73% higher sperm count than those who exercise for less than 5 hours a week.
- Smoking: A study published in Environmental Epidemiology found a strong association between smoking and lower semen volume and total sperm count in fertile men.
- Processed diets: According to research published in JAMA Network Open, men who consume a Western diet, pizza, fries, sweets, sodas, and red and processed meats, typically have a lower sperm count and lower levels of reproductive hormones needed for optimal fertility.
- Endocrine disruptors: Endocrine disruptors are chemicals that disrupt the hormones in the body, causing a number of hormone-related health issues, one of which includes poor sperm count. A study published last year found that exposure to products known to contain endocrine disruptors can affect semen volume and total sperm count per ejaculation.
What are the dangers of low sperm count?
Aside from making it more difficult to conceive, there are other health issues associated with low sperm count.
In 2018, a study focused on Italian men found that those who had a low sperm count were 1.2 times more likely to have more body fat, higher blood pressure, higher bad cholesterol and triglycerides, and lower levels of good cholesterol. All of these factors can increase the risk of chronic conditions such as heart disease, hypertension, and diabetes.
Additionally, a study published in Fertility and Sterility found an association between poor semen quality and an increased risk of testicular cancer.
How can we improve sperm count?
The Mayo Clinic suggests the following ways to improve sperm count:
- Maintain a healthy weight
- Eat a healthy diet
- Engaged in safe and protective sex
- Manage stress.
- Exercise
- Quit smoking
Takeaway
The recently published review does put a spotlight on the potential threat to men’s reproductive health. However, not everyone is convinced. Some experts believe that since the manner in which sperm is counted has changed so much over the years, it’s hard to fully accept the study’s findings.
In any case, it is still important to highlight these types of studies so that men can make better-informed choices for their health.
MAIN IMAGE CREDIT: Arthit Premprayot/Shutterstock
References
Andersen, E., Juhl, C. R., Kjøller, E. T., Lundgren, J. R., et al. (2022). Sperm count is increased by diet-induced weight loss and maintained by exercise or GLP-1 analogue treatment: a randomized controlled trial. Human reproduction (Oxford, England), 37(7), 1414–1422. https://doi.org/10.1093/humrep/deac096
Hanson, H. A., Anderson, R. E., Aston, K. I., Carrell, D. T., et al. (2016). Subfertility increases risk of testicular cancer: evidence from population-based semen samples. Fertility and sterility, 105(2), 322–8.e1. https://doi.org/10.1016/j.fertnstert.2015.10.027
Istvan, M., Rahban, R., Dananche, B., Senn, A., et al. (2021). Maternal occupational exposure to endocrine-disrupting chemicals during pregnancy and semen parameters in adulthood: results of a nationwide cross-sectional study among Swiss conscripts. Human reproduction (Oxford, England), 36(7), 1948–1958. https://doi.org/10.1093/humrep/deab034
Levine, H., Jørgensen, N., Martino-Andrade, A., Mendiola, J., et al. (2022). Temporal trends in sperm count: a systematic review and meta-regression analysis of samples collected globally in the 20th and 21st centuries. Human reproduction update, dmac035. Advance online publication. https://doi.org/10.1093/humupd/dmac035
Levine, H., Jørgensen, N., Martino-Andrade, A., Mendiola, J., et al. (2017). Temporal trends in sperm count: a systematic review and meta-regression analysis. Human reproduction update, 23(6), 646–659. https://doi.org/10.1093/humupd/dmx022
Nassan, F. L., Jensen, T. K., Priskorn, L., Halldorsson, T. I., et al. (2020). Association of Dietary Patterns With Testicular Function in Young Danish Men. JAMA network open, 3(2), e1921610. https://doi.org/10.1001/jamanetworkopen.2019.21610
Sermondade, N., Faure, C., Fezeu, L., Lévy, R., Czernichow, S., & Obesity-Fertility Collaborative Group (2012). Obesity and increased risk for oligozoospermia and azoospermia. Archives of internal medicine, 172(5), 440–442. https://doi.org/10.1001/archinternmed.2011.1382
Tang, Q., Pan, F., Wu, X., Nichols, C. E., et al. (2019). Semen quality and cigarette smoking in a cohort of healthy fertile men. Environmental epidemiology (Philadelphia, Pa.), 3(4), e055. https://doi.org/10.1097/EE9.0000000000000055


![women [longevity live]](https://longevitylive.com/wp-content/uploads/2020/01/photo-of-women-walking-down-the-street-1116984-100x100.jpg)










