Tuesday, 21 September, is World Alzheimer’s Day – a day in which organisations around the world focus their efforts on raising awareness for Alzheimer’s and dementia. Every three seconds, someone in the world develops dementia. The WHO Global status report 2021 indicates that as many as 139 million people could be suffering from dementia by 2050 (an increase from 55 million in 2019)[1].
Alzheimer’s, the most common form of dementia, is a general term for memory loss and the impairment of other intellectual abilities that are serious enough to interfere with daily life. It accounts for 50 to 80 percent of dementia cases[2].
What is dementia?
Dementia is a term used to describe a group of symptoms caused by different disorders and conditions that leads to the deterioration of a person’s ability to remember, communicate or make decisions.

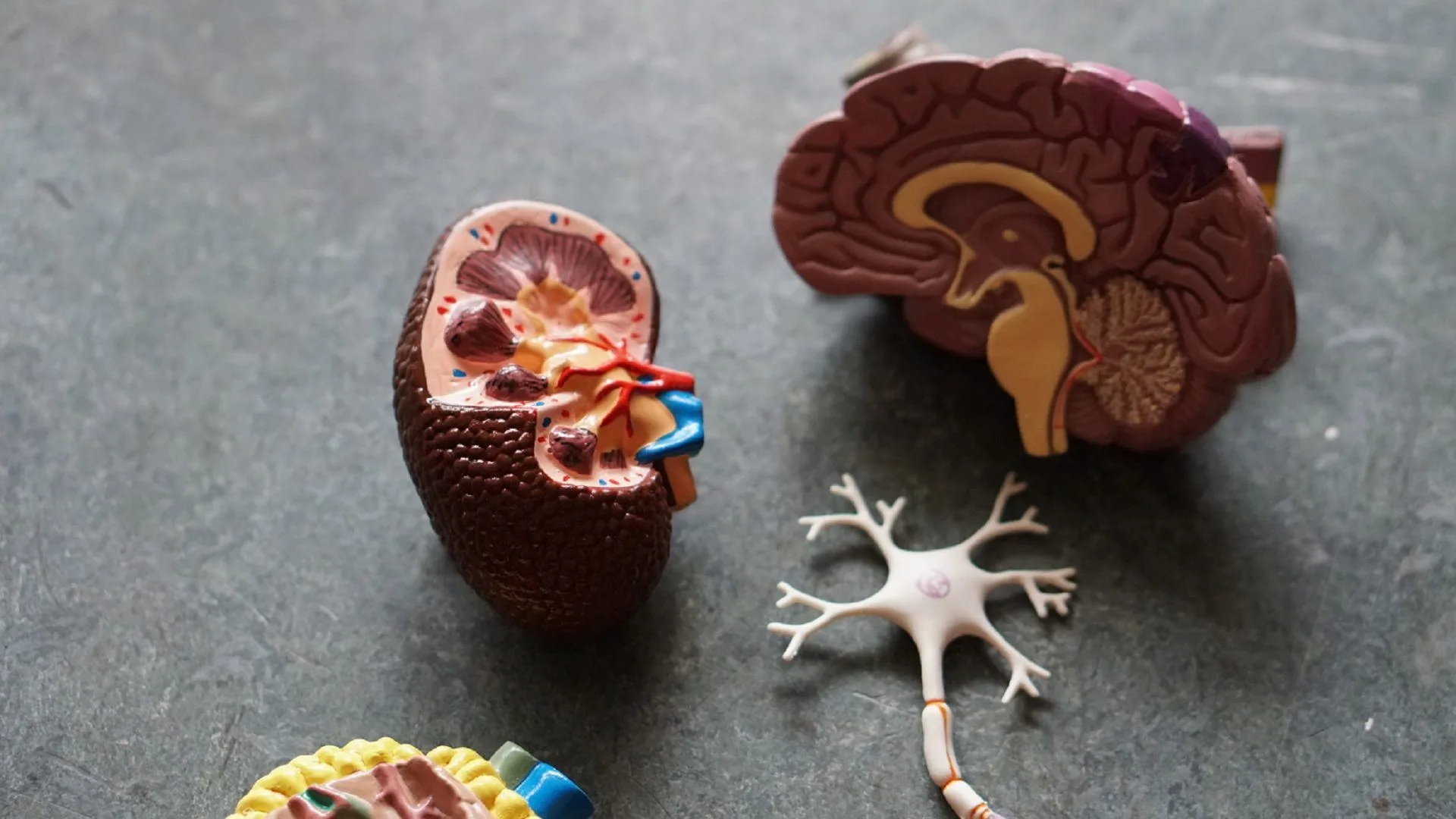
Lightspring/Shutterstock
Whilst the exact cause of the disease is unknown, it is known to be both progressive and incurable. Over time, the brain will continue to deteriorate, impacting the person’s daily performance until they are no longer able to function and lose the ability to lead a normal life.
Although certain prescribed medications can slow the progression, this is only possible for a certain length of time. It is actually very difficult to get an exact and final diagnosis, with a true diagnosis only possible after a post-mortem has been conducted. Early diagnosis is usually made clinically (presenting facts) rather than medically (tests).
The first step in a clinical diagnosis will usually entail ruling out any other diseases (constipation, UTI, temperature, pneumonia, very low blood pressure, dehydration, stroke, low folic acid levels, lack of vitamins, brain tumour, stress, trauma) as a probable cause for the symptoms being experienced.
Symptoms
Certain symptoms exhibited in the early stages of the disease could also look similar to the natural aging process. It is a difficult and complex process, and it is highly recommended to involve a specialist such as a psychiatrist or a neurologist. The family also has a very important role to play in the diagnosis, as they know both present and past information about the person.
While signs and symptoms of Alzheimer’s differ from person to person, Alzheimer’s is usually characterized by four stages: mild, moderate, severe, and terminal.
Mild

Lightspring/Shutterstock
Symptoms begin slowly and are usually mild and can be hidden. This is why most people are not diagnosed until the moderate stage. Loss of short-term memory is usually one of the most common symptoms at this stage.
Moderate
The person is often aware that something is wrong and may ask for help. In this stage, the patient may need more help and frequent reminders to help them cope with daily living. The person may also become very upset or angry and aggressive, as they may feel frustrated that they are not able to do things for themselves as they did before.
Severe
At this stage, people are not aware of their memory changes and usually cannot complete even simple or routine tasks and will become increasingly frail.
Terminal
Often at this stage, the patient requires constant care. Communication is minimal and often non-existent. The person is unable to help him or herself even in the smallest way. Some people never reach this stage.
Helping people with dementia
I outline some of the things that can be done in order to help a person suffering from dementia. These include:
-
Stick to a regular daily routine. Make sure there are lots of familiar objects around to be seen and enjoyed.
-
Regularly check on the patient’s safety.
-
Make sure the patient eats well and drinks plenty of fluids.

Lightspring/Shutterstock
-
Help the patient remain as independent as possible for as long as possible.
-
Provide regular exercise and recreation.
-
Keep in touch with friends and family.
-
Use written memory aids such as large calendars and clocks, written lists of daily routines, reminders about safety measures, and name tags placed on important objects.
-
Ensure that the patient gets regular medical check-ups.
-
Plan for future needs, such as respite care or nursing home placement.
-
Provide lots of emotional support to the patient and all the caregivers.
-
If medication is prescribed, see that the patient takes it regularly.
-
Join a support group of other people who care for people with dementia.
-
Ask for help with money problems, legal problems, day-to-day advice, emotional issues, respite care, or nursing home placement when they are needed.
-
Check the home for safety features such as bars on the wall near the toilet and bathtub, night lights in hallways and on the stairs, non-slip rugs, lowering the height of the bed to prevent falls, lowering the temperature of the geyser water, putting bells on all external doors so that you can hear if the patient is going outside, etc.
-
Make sure all health care providers have a complete list of all the patient’s prescriptions and over-the-counter medicines.
-
If incontinence is a problem, remind the patient to use the toilet every two hours.
-
Enrol the patient in a dementia day programme to provide stimulation for the patient and respite for the caregiver.
A family disease
 Alzheimer’s, and dementia in general, can be an incredibly difficult and emotionally distressing experience, particularly for the patient’s loved ones and family members.
Alzheimer’s, and dementia in general, can be an incredibly difficult and emotionally distressing experience, particularly for the patient’s loved ones and family members.
Often known as a ‘family disease’, dementia not only affects the patient but has an enormous impact on their family and friends as well.
A patient, particularly in the more advanced stages of the illness, may not be aware of how ill they are. There is kindness in this. However, the patient’s reality can often be very different from the reality of their family and loved ones.
The family of the patient is acutely aware of, and witness to, the gradual deterioration of their loved one. It can take as long as 10 to 15 years from initial diagnosis until the eventual passing of the patient. The last five years often see the patient admitted to an old age home or care facility.
This is an extraordinarily long and cruel grieving process during which time family members may experience a range of emotions from loss and grief through to guilt, anger, embarrassment, sadness, and eventually, even relief. It is vital that family members and loved ones of a patient diagnosed with Alzheimer’s allow themselves access to their own care and support during this time.
A combination of a social worker, counsellor, and support groups can play a huge role in aiding the family members to process their own loss and emotions, helping to provide structures and tools that allow them to be able to continue with their own lives during these difficult years and eventually, with time, to be able to let go.
Alzheimer’s Disease Early Warning Signs
- A memory problem that is NOT caused by alcohol abuse or head injury, and which worsens with time.
- Language problems. Difficulty naming objects, finding the right word to use in a sentence, and often speaking nonsense.
- Zips and buttons are difficult to fasten. Alzheimer’s sufferers find it hard to dress.
- H Those with Alzheimer’s may not care about how they look and may not want to bathe.
- Extreme mood swings. A change in mood for no reason – going from calm to suddenly scared or angry and aggressive within minutes.
- Impaired judgment. Strange behaviour – like wearing underclothes over outer garments or taking clothes off in public.
- Many Alzheimer’s sufferers get lost in familiar places, such as their own neighbourhood.
- Even recognition of their own family and friends becomes difficult.
- Recalls memories of childhood at times, but cannot remember anything that happened the same day.
- Suspicious of other people and may accuse them of stealing or hiding things.



![women [longevity live]](https://longevitylive.com/wp-content/uploads/2020/01/photo-of-women-walking-down-the-street-1116984-100x100.jpg)










