Crippled with fatigue and alarmed at heart palpitations that seemingly come from nowhere, millions around the world are slogging through long Covid, an aftermath illness that can go on for months. However, long Covid does not have to be a life sentence.
In for the long haul
Chances are you know someone with long haul Covid – it may affect as many as 35% of all those infected by the novel coronavirus. That’s according to the chief medical adviser to the US president, Anthony Fauci, quoted earlier this year. Other studies have put it closer to 10% of cases. Whichever is accurate, questions outnumber answers, such as “Why do my toes tingle”? Yes, “COVID toes” is a phenomenon, if not the most common one.
The Big Deal With Long Covid
If the 10% estimate is correct, then 20+ million people around the world may suffer from long Covid. Currently, worldwide COVID-19 cases exceed 219 million on the Johns Hopkins dashboard.
Just like one of the most common symptoms – brain fog – a murkiness hangs over understanding this protracted illness, and the US NIH (National Institutes of Health) has announced a project to get to grips with it.
That’s thanks to Congress approving US$1 billion funding to arrive at clarity and a way forward that eludes patients and caregivers today.
Yes, finally the experience of ‘long haulers’ is being taken more seriously than before. Initially, many patients were met with skepticism. Women, in particular, complained about being fobbed off and dismissed because their symptoms seemed psychological. But the current data shows it’s clear that symptoms are real – not “just anxiety” or “in people’s heads”.
Months after having COVID-19, millions haven’t returned to their pre-infection health. The intensity of the experience varies, but many battles with basic activities, let alone working a full day. Long Covid can be as frustrating as it is debilitating because there’s so much we don’t know.
What It Is
The UK’s National Institute for Health and Care Excellence (NICE) says the name Long Covid is given to describe the myriad symptoms that develop or continue after acute COVID‑19, 4 weeks or more after the initial infection.

Photo by Kelly Sikkema on Unsplash
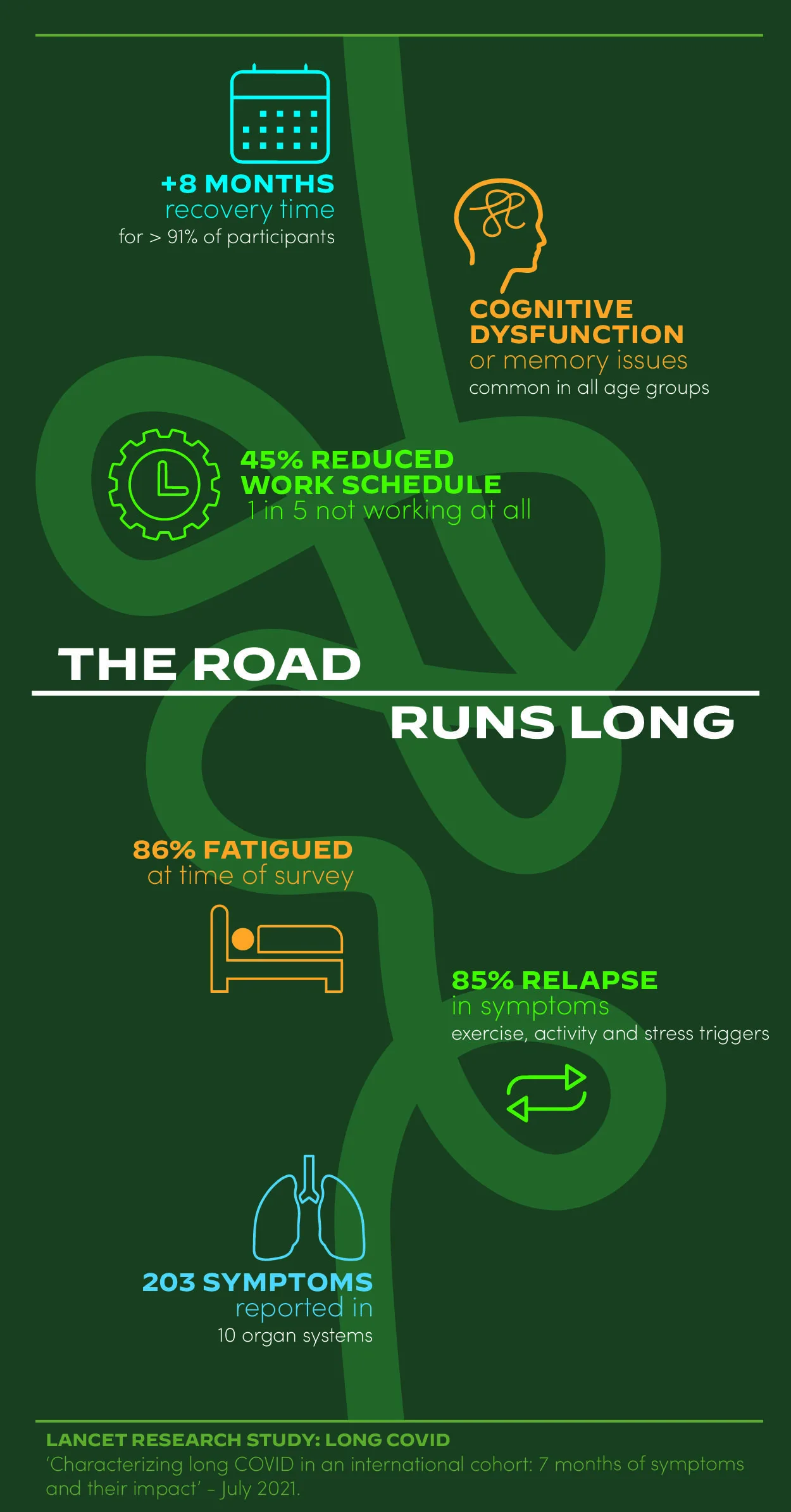
Arguably the broadest study of Long Covid comes from Lancet, published on 15 July 2021. The research includes more than 3,000 people from 56 countries with illnesses lasting more than 28 days. This study confirms what others have found:
Long Covid has a clutch of common symptoms with a long tail. Over 200 symptoms have been detected, affecting 10 organ systems.
Symptoms
The Lancet study finds the 3 most common symptoms to be fatigue, post-exertional malaise, and cognitive dysfunction. This reflects what patients describe in their own words as a brain fog that won’t lift.
Other common symptoms include shortness of breath, persistent cough, muscle and joint pain, sleep disturbances, migraines, skin rashes, and new sensitivities to smell and taste. Chest pain and dysautonomia, usually a rare condition, are reported regularly. The latter may include a racing heart. To honor the real experience: it freaks people out.
Looking further into research isn’t pretty, either – critical bodily functions are affected, which include cardiovascular, nervous, brain, and respiratory systems.
When patients relapse, it’s often a triple-wave experience, where Wave 1 starts with a dry cough and fever. Wave 2 brings on symptoms like heart palpitations peaking after two months, then tapering. Wave 3 is reported to start about a month after the initial infection and people report skin rashes, muscle pain, new allergies, and brain fog. Unfortunately, symptoms can remain for months afterward, even a year in some instances. It’s hardly surprising that depression, anxiety, and stress weigh heavily. Yes, it might also be in our heads, with good reason.
Seemingly unrelenting symptoms aside, what is the general prognosis? Doctors offer hopeful anecdotes that most will recover without life-limiting damage. As a counterpoint, other sources sound a more serious note.

Photo by Brittany Colette on Unsplash
The Long-Term Effect Of Long Covid
The current timeframe means that scientists don’t conclusively understand long-term effects, but Mayo Clinic already reports concerning indicators :
-
Lungs
COVID-19 is known primarily for hitting the lungs, and pneumonia associated with COVID-19 suggests long-standing damage to air sacs (alveoli) in the lungs. UC Davis says “Some patients who have been seriously ill from COVID-19 develop acute respiratory distress syndrome (ARDS), which can permanently scar their lungs”.
-
Brain
Strokes, seizures, dementia, and Guillain-Barre syndrome (temporary paralysis) are all linked to COVID-19. Amy Proal, a microbiologist at PolyBio Research Foundation, says that infectious organisms can contribute to brain disease [4]. She says that SARS-CoV-2, like other viruses, can get into brain nerves and stay there. This may be a link to brain fog and loss of taste and smell.
-
Heart
The risk of heart failure or other heart complications may occur down the line. Heart damage caused by COVID-19 is likely due to small clots in tiny blood vessels (capillaries) in the heart muscle. The virus can also weaken blood vessels, causing them to leak, resulting in long-lasting liver and kidney problems.
-
Senses
Many people worry that long-term loss of smell and taste may be permanent. Christian Sandrock, professor of pulmonary and critical care medicine at UC Davis Health, believes that the loss of smell and taste won’t last forever: “For most people, there will likely be a resolution, but there isn’t a clear answer as to how long this will take”.
-
Prolonged fatigue
This is a curious thing that has caught the attention of many, including Anthony Fauci, who is quoted as saying symptoms like brain fog and fatigue are “highly suggestive” of myalgic encephalomyelitis (ME) or chronic fatigue syndrome (CFS). This is not the first time that ME has been observed as a post-viral malady.

Photo by Andrea Piacquadio from Pexels
A Crisis Of Fatigue
Long Covid seems to support a prior theory that ME/CFS begins with an infection. Mady Hornig (MD, Columbia University Medical Center’s epidemiology faculty), reports that about 75% of ME diagnoses are caused by Epstein-Barr virus (EBV). EBV is a herpes virus, but Hornig is speculating that SARS-CoV-2, might trigger EBV and hence fatigue.
Not wanting to waste a good crisis, Mady Hornig says that researching so many Long Covid cases is an opportunity to help millions who already battle with ME and chronic fatigue.
Others like Hornig think it’s possible that our autonomic nervous system is acting up since it governs heart rate, blood pressure, respiration, and digestion. This will reveal a link to that unnerving symptom long haulers experience: tachycardia (racing heart). If you’ve heard of POTS (postural orthostatic tachycardia syndrome) this is a disorder of the same body system and once again brain fog and fatigue are common. According to Mitchell Miglis (Stanford University neurologist), it may turn out that POTS, ME/CFS, and persistent COVID-19 are the same thing. It’s just that doctors in different areas of specialism call them by different names.
Who Takes The Hit?
Just as there are three waves of symptoms, there seem to be three surprises in the profile of long haulers:
|
1 |
2 |
3 |
|
Mild symptoms with the primary COVID-19 infection. What really foxes the medical world is that people with persistent long-haul symptoms were generally not severely ill with the acute COVID-19 [12]. |
Around 40 years old. University College London Hospitals (UCLH) reports that the 35-49 age group is the most affected. This is surprising because this cohort was considered to be resilient with ordinary COVID-19. |
Women with no relevant medical history. Women outnumbered men 4 to 1 with Long Covid at a Paris hospital during the course of 2020 [10]. No reason is known why women seem more susceptible. |

Photo by EVG Culture from Pexels
Three Possible Causes
There are three theories of causation that are increasingly publicized.
1. Other latent viruses are activated because the immune system is weak.
As the coronavirus damages or de-conditions the immune system it’s possible that other dormant viruses ‘wake up’ and harm the body. This is the theory where, for example, the likes of a herpes virus is activated, triggering symptoms of fatigue.
2. Autoimmunity continues in override mode
In this scenario, immune systems overreact and stay in this state even once the infection is over. This causes chronic inflammation because the immune system attacks healthy cells by mistake, damaging various body tissue. A rare multi-system inflammatory syndrome (MIS) can also occur with COVID-19. In this condition, various organs become inflamed.
3. The virus remains hidden in parts of the body
Small amounts of pathogens survive in remote areas of the body where the immune system can’t reach them. This may be part of the reason that many post-infection issues occur. Not unique to COVID-19, this may hold true for other fatigue illnesses like ME.
The body is such a complex system that many permutations are possible. Some good news is that the threat for children is not as great as initially thought, as the BBC reports.
Are long haulers contagious?
Since good news is rare, here’s another reason to take heart: “We’re pretty clear that patients who are symptomatic for four months are probably not contagious. But when they stop being contagious is not clear” says Sandrock.
What To Do
- Keep up good habits
Hackneyed as they may be, the proven ways to mitigate risk are masking, social distancing, crowd avoidance, hand washing, and vaccination.
Vaccination can help prevent people from contracting the virus and developing Long Covid in the first place.
- Prevent with wellness
We’re always banging this drum and it seems as valid as ever. If we know anything, long Covid is a dreadful experience, and every effort to avoid it is worthwhile.
Returning to exercise requires great caution. Pay attention to how you feel and be careful if you have any respiratory or cardiac issues.
Other basic pillars of wellness (healthy diet, stress reduction, and sleep) seem appropriate.
As part of a healthy diet, we’re keeping up our daily regime of Moksha Lion’s Mane mushrooms. Lion’s Mane has been researched as a very low/no-risk supplement for reducing inflammation, gastric health, promoting brain nerve growth, and mental clarity. Nonetheless, it has not been researched for long Covid and this is not a recommendation to diagnose, treat, cure, or prevent it.
- Stay the course and manage symptoms as best you can
BMJ, a global healthcare knowledge provider, reports “Many patients recover spontaneously (if slowly) with holistic support, rest, symptomatic treatment, and gradual increase in activity”.
- Seek qualified help
Clinicians suggest that if you have new, persistent, or progressive symptoms that are respiratory, cardiac, or neurological, then it’s wise to consult a doctor or a specialist in that field.
Community At Hand
Medical centers and online support groups have been popping up in the last 12 months. These are among the prominent ones, but there are others, too.
- The Body Politic COVID-19 Support Group provides emotional support, resources, community, and opportunities for advocacy. They’re active on Instagram, Twitter, and Youtube.
Their Patient Led Research Collaborative is now in a second survey of antibody testing results, neurological, cardiovascular, systemic symptoms, and mental health.
- COVID-19 Survivor Corps is a grassroots movement “connecting, supporting, educating, motivating and mobilizing COVID-19 Survivors”
- You + ME Registry and Biobank is an online clinical study of individuals committed to identifying a cure for myalgic encephalomyelitis (ME or chronic fatigue syndrome), Long Covid, and other post-viral illnesses.
- Covid Watch, a Penn Medicine outreach program, checks in with patients at risk for complications of COVID-19 who are self-isolating at home.
- Clinics that treat long haulers include New York’s CORE clinic at Montefiore Medical Center, California’s Cedars-Sinai’s Recovery Program, and Cleveland Clinic’s Post-ICU Recovery Clinic.
Final Word
Most people with COVID-19 recover quicker than the cases mentioned here, but to all those slogging it out, here’s to your recovery. As long and frustrating as the road may be, recent data suggests long haulers are regaining their health. Scientists, researchers, and medical professionals the world over are working tirelessly to get to grips with this ubiquitous virus and its aftermath. It may be a long road, but you have smart and dedicated people on your side. May we all look forward to a healthier, happier future.
Main photo credit: Photo by Hari Panicker on Unsplash
Sources
- https://www.ama-assn.org/delivering-care/public-health/dr-fauci-offers-2021-forecast-covid-19-vaccines-treatments
- https://www.aad.org/public/diseases/coronavirus/covid-toes
- https://www.healthline.com/health-news/long-haul-covid-19-symptoms-may-appear-in-this-order#Symptoms-that-come-in-waves
- https://www.bbc.com/future/article/20210609-how-long-will-long-covid-last
- https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-long-term-effects/art-20490351
- https://health.ucdavis.edu/coronavirus/covid-19-information/covid-19-long-haulers.html
- https://health.ucdavis.edu/health-news/coronavirus/the-frightening-uncertainty-for-long-haul-covid-19-patients/2020/12
- https://www.meaction.net/2020/07/10/dr-anthony-fauci-says-that-post-covid-syndrome-is-highly-suggestive-of-myalgic-encephalomyelitis/
- https://jamanetwork.com/journals/jama/fullarticle/2771111
- https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(20)30436-5/fulltext
- https://www.frontiersin.org/articles/10.3389/fmicb.2021.724654/full
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/covid-long-haulers-long-term-effects-of-covid19
- https://www.bmj.com/content/370/bmj.m3026




![women [longevity live]](https://longevitylive.com/wp-content/uploads/2020/01/photo-of-women-walking-down-the-street-1116984-100x100.jpg)










