Multiple organ failure is a hallmark of sepsis, and recent research has uncovered its progressive phases. In the first phase, known as the “cytokine storm,” an out-of-control cytokine reaction causes symptoms including high body temperature and respiratory failure. Longevity Live Paid Content.
It is not always possible to eradicate sepsis with compounds that lower hypercytokinemia by lowering levels of cytokines, especially tumor necrosis factor (TNF). There have been over 40 clinical studies of options for reducing the proinflammatory response, and none have shown any positive outcomes.
Researchers observed that in animal research studies observing the potential impact of Thymalin peptide on organ failure noted: “giving these mice Thymalin lowered their fever, slowed down cell death, increased the number of cells in their spleen, lowered the production of cytokines, and increased the activity of the signaling pathways that were studied.”
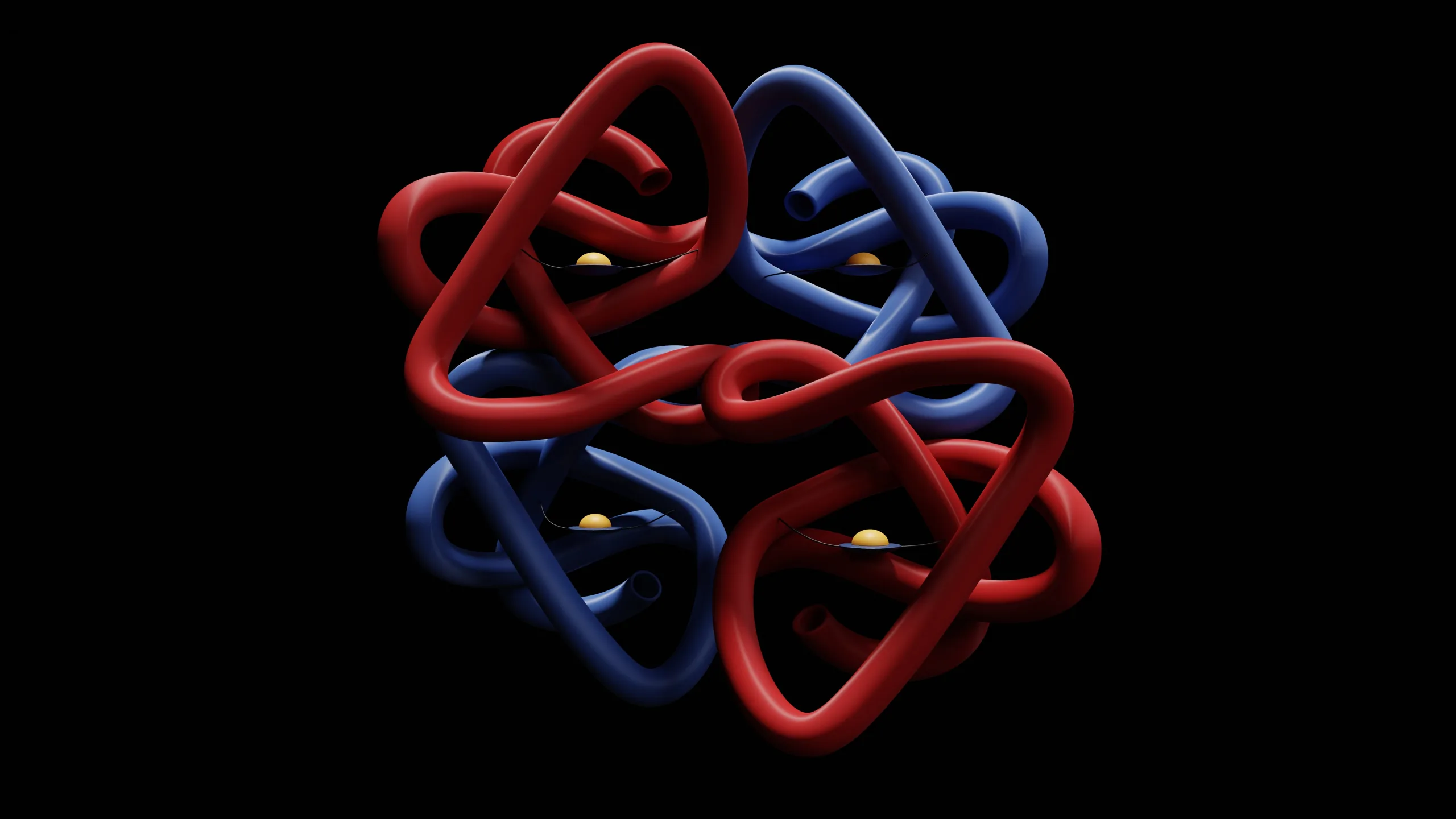
By eliminating immune cells, apoptosis helps keep the immune system in balance. The transcription factor NF-B turns on the transcription of genes that either help cells die or stop them from dying. The caspase family of cysteine proteases cuts proteins in cells. Apoptosis of cells of the adaptive immune system is induced in tandem with caspases, which is ironic given that NF-B drives hyperinflammatory responses by boosting cytokine production. Studies on animals with severe sepsis suggest more apoptosis during the “cytokine storm” stage, which is marked by a sharp drop in the number of T, B, and dendritic cells.
What happens during a cytokine storm?
It was thought that after LPS treatment, the levels of IL-6, IFN-β, and TNF-β in the plasma would rise because the NF-B and MAPK pathways control their production. There was also an increase, although not as dramatic, in plasma levels of the anti-inflammatory cytokine IL-10. Findings implied that Thymalin presentation, either free or attached to nanoparticles, appeared to totally restore proinflammatory cytokine levels.
Further research results suggested that when mice that are prone to inflammation were given the thymic peptide Thymalin, their bodies seemed to make less of the heat shock protein Hsp70 and pro-inflammatory cytokines.
Scientists speculate that plasma levels of IL-1, IL-2, IL-6, TNF-, interferon-, and IL-10, a cytokine that fights inflammation, appeared to go up when LPS caused inflammation. It has been hypothesized that giving Thymalin beforehand may have reduced the buildup of inflammatory cytokines in the blood. Additionally, Thymalin seemed to have stopped spleen lymphocytes and peritoneal macrophages from making more cytokines when LPS was present. When Thymalin was added to macrophages that had been stimulated by LPS in a culture, the cells appeared to make less TNF-α at their peak. The peak of LPS-induced Hsp70 synthesis was also reduced by Thymalin, studies suggest.
Thymalin Peptide and Immune Suppression
Researchers have also noted that “the first stage of a cytokine storm that gets out of hand always throws the immune system out of whack. This makes it more likely that subjects will get a secondary infection like pneumonia or a latent herpes virus (including cytomegalovirus) infection that comes back to life.”
Studies conducted over the last decade have suggested that sepsis causes hyperinflammation, decreased immunity, and even failure of the adaptive immune system. The development of severe immunodeficiency is seen as the major reason for the failure of sepsis treatment by some researchers and clinicians.
When Thymalin was given to old mice, the amount of FTS in their blood, the number of CD4+ cells in their bone marrow, and the amount of corticosterone in their blood all appeared to go up. “Both natural and synthetic pharmaceuticals changed the mixture of cyclic nucleotides and cytokines [interleukin (IL)-2, interferon (IFN)] released by blood lymphocytes. They also increased T-cell differentiation and T-cell recognition of peptide-MHC complexes.”
An alternative compound that has also garnered interest from researchers is Zinc. Zinc is required for T-cell proliferation, development, and differentiation. Thymalin is a well-known zinc-dependent thymic hormone that plays a critical role in T-cell development and occurs in two forms: an active one that is zinc-bound and an inactive one that is zinc-free. Zinc may also stop the programmed death (apoptosis) of precursor T-cell populations and mature CD4+ T cells by affecting several enzyme processes and the ongoing production of glucocorticoids. Enhancing antibody synthesis in older mice, restoring antibody avidity in elderly or thymectomized animals, and inhibiting hyperalgesia after injury in mice and rats are all hypothesized properties of Thymalin peptide.
Thymalin Peptide and Fibrosis
Studies suggest that Thymalin may promote anti-inflammatory cytokines while suppressing pro-inflammatory ones. It has been hypothesized to inhibit NF-kappaB activation, which plays a significant pathogenic role in various lung illnesses, and downregulate p38, which is involved in glucocorticoid tolerance.
Study results suggest that in alveolar epithelial cells that were presented with Thymalin, RelA (p65) appeared lowered. RelA is the main member of the NF-kappaB family that turns on other proteins. Zn (2+) only slightly supported this effect. Research suggests the DNA-binding activity of NF-kappaB (RelA/p65) also seemed inhibited by Thymalin/Zn(2+), and this effect seemed concentration-dependent. These findings suggest that Zn(2+) may synergistically enhance the anti-inflammatory impact of Thymalin, which is mediated via cAMP, by downregulating the production of proinflammatory cytokines, notably IL-1 beta. Understanding the anti-inflammatory-relieving potential of Thymalin requires an appreciation for the molecular control of Thymalin via an NF-kappaB-dependent pathway. Furthermore, Thymalin decreased bleomycin-induced cytokine and chemokine production and prevented pulmonary fibrosis in mice. Haddad et al. suggested that Thymalin may act as an immunomodulator in the perinatal epithelium of the lung.
References
- Lunin, S.M., Khrenov, M.O., Novoselova, T.V., Parfenyuk, S.B. and Novoselova, E.G. (2008). Thymulin, A Thymic Peptide, Prevents the Overproduction of Pro-Inflammatory Cytokines and Heat Shock Protein Hsp70 in Inflammation-Bearing Mice. Immunological Investigations, 37(8), pp.858–870. https://www.tandfonline.com/doi/full/10.1080/08820130802447629
- Novoselova, E.G., Lunin, S.M., Glushkova, O.V., Khrenov, M.O., Parfenyuk, S.B., Zakharova, N.M. and Fesenko, E.E. (2018). Thymulin, free or bound to PBCA nanoparticles, protects mice against chronic septic inflammation. PLOS ONE, 13(5), p.e0197601. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197601
- Morozov, V.G. and Khavinson, V.K. (1997). Natural and synthetic thymic peptides as therapeutics for immune dysfunction. International Journal of Immunopharmacology, [online] 19(9), pp.501–505.
- Labunets, I.F., Rodnichenko, A.E., Magdich, L.V. and Butenko, G.M. (2012). The thymus and adaptive changes in the cellular composition of bone marrow in animals of different ages. Advances in Gerontology, 2(1), pp.27–34.
- Santos, M., Henriques-Coelho, T. and Leite-Moreira, A. (2010). Immunomodulatory role of thymulin in lung diseases. Expert Opinion on Therapeutic Targets, [online] 14(2), pp.131–141. Available at: https://www.ncbi.nlm.nih.gov/pubmed/20055713
Who is the author?

Aleeha Khan
Aleeha Khan is a dedicated Content Writer in Peptides with a passion for translating complex scientific information into engaging and accessible content.
She is proficient in conveying the latest advancements, benefits, and applications of peptides in various fields. She is also committed to fostering understanding and awareness through informative and compelling writing.



![women [longevity live]](https://longevitylive.com/wp-content/uploads/2020/01/photo-of-women-walking-down-the-street-1116984-100x100.jpg)