Antibiotics that are designed for human use have been used in farming over the years to help animal lots grow faster and larger thereby increasing the yield for farmers. This boosts farm to plate efficiency and profitability. It has been estimated that animals who are injected with or fed antibiotics grow about twice as fast as those who are grass-fed. In addition, explains Angus McIntosh, a bio-dynamic farmer based in Stellenbosch, South Africa, antibiotics are especially good at killing bacteria, both good and bad. This comes in handy when it comes to concentrated feeding operations where animals are kept in small spaces and live in close proximity to their excrement.
Why is this a problem?
Over-use of chemical antibiotics is leading to a phenomenon known as antibiotic resistance. In humans, antibiotic resistance is growing at an alarming rate and this is of concern to health authorities.

hlphoto/shutterstock
Indeed, the World Health Organization calls antibiotic resistance one of the biggest threats to global health, food security, and development today. As a result of this issue, doctors are finding it increasingly hard to treat a growing number of infections, including pneumonia, TB, salmonellosis, and gonorrhea. It also leads to longer hospital stays, higher medical costs, and increased mortality.
According to the American Centers for Disease Control and Prevention, it is already causing some 23 000 deaths and $34 billion losses every year in the US.
How is this issue regulated?
In January 2017, the FDA introduced rules about the use of human antibiotics purely for growth promotion in animals, and steps were taken to ensure the encampment of antibiotic resistance. However, it seems there is difficulty in getting full compliance from farmers and vets.
A recent report in The New York Times highlighted the plight of Sandy Lewis, an organic cattle farmer in upstate New York who bought 13 bulls from a breeder in Oklahoma. After a few of these animals died under violent circumstances, he discovered that the herd had been infected by anaplasmosis.

Photo by Andrey Niqi from Pexels
This is a bacterial illness that destroys red blood cells and deprives the animals of oxygen, causing them at times to act violently. The disease is relatively rare in the Northeast, yet according to the report, a quarter of Mr. Lewis’s own herd ended up becoming infected. He spent more than $100,000 trying to save the rest. Ultimately, another 100 animals had to be culled. After a two-year investigative journey into the use of antibiotics animals, Mr. Lewis spoke out to the New York Times questioning, “Are pig, cattle and poultry farmers misusing antibiotics, allowing too much of the drug to get into our food?
It has long been common knowledge in the agricultural sector that antibiotics can help cause animals to grow fatter faster. Time is money, particularly in the food industry, and for many years ranchers used antibiotics not just for treating diseases, but also for promoting growth so that animals would be ready for the slaughterhouse sooner. (Mr. Lewis told the New York Times that his grass-fed steers require 27 months to get to market without antibiotics, more than twice as long as it takes cows pumped full of antibiotics.)
Indeed, back in 2014, the New York Times reported that there were already some concerns around antibiotic use in farming. An opinion piece written by Pagan Kennedy alluded to “decades of agricultural research which has shown that antibiotics seem to flip a switch in young animals’ bodies, helping them pack on pounds.” In other words, the drugs act like a kind of superfood to produce cheap meat. Medical investigators were considering the role antibiotics might play in encouraging the same growth promotion in humans. There was evidence that America’s growing obesity epidemic was connected to these drugs.

Gregory Gerber/Shutterstock
Fast forward to today, and antibiotics are back in the spotlight for a different reason. Antibiotic resistance is an epidemic of global and potentially devastating consequences. According to a study published in the journal Frontiers in Microbiology, this is becoming a global challenge. Antibiotics are starting to be considered an “endangered species” facing extinction due to the worldwide emergence of antibiotic resistance (ABR).
What if this resistance is aided and abetted by the meat we are eating? Agreed, we receive our greatest exposure in the pills we take, rather than the food we eat. However, given the rising concerns around antibiotic abuse, surely it is important that people are aware their food may well contain high traces of these drugs?
Why should you care?
Dr. Martin, J. Blaser, is the former president of the Infectious Diseases Society of America and an expert on the human microbiome. He has some explanations based on many years of data collection and research. In “Missing Microbes. How the Overuse of Antibiotics is Fuelling Our Modern Plagues,” he shed light on the human microbiome.
The human microbiome is the collection of bacteria, viruses, fungi, and other microbes that live in and on the body. Indeed, up to 90 percent of all the cells in the human body aren’t human at all — they’re micro-organisms. Dr. Blaser and his colleagues at the Blaser Lab spent years studying the effects of antibiotics on the growth of baby mice. In one experiment, he lab-raised mice on both high-calorie food and antibiotics.

Lynn2511/Shutterstock
The results of the study were dramatic, particularly in female mice: They gained about twice as much body fat as the control group mice who ate the same food. “For the female mice, antibiotic exposure was the switch that converted more of those extra calories in the diet to fat, while the males grew more in terms of both muscle and fat.”
In his book, he explains that their observations were consistent with the idea that the modern high-calorie diet alone is insufficient to explain the obesity epidemic and that antibiotics could be contributing. The Blaser lab also investigated whether antibiotics may be changing the animals’ microbiome — the trillions of bacteria that live inside their guts. These bacteria seem to play a role in all sorts of immune responses, and, crucially, in digesting food, making nutrients, and maintaining a healthy weight.
And antibiotics can kill them off.
Dr. Blaser told National Public Radio that when he launched his book, “since World War II, we’ve seen big rises in a number of diseases: asthma, allergies, food allergies, wheat allergy, juvenile diabetes, obesity…These are all diseases that have gone up dramatically in the last 50 or 70 years. One of the questions is: Why are they going up? Are they going up for 10 different reasons, or perhaps there is one reason that is fuelling all of them. My theory is that the one reason is the changing microbiome; that we evolved a certain stable situation with our microbiome and with the modern advances of modern life, including modern medical practices, we have been disrupting the microbiome. And there’s evidence for that, especially early in life, and it’s changing how our children develop.”
Simply put, antibiotic abuse over time interferes with your microbiome because antibiotics cannot differentiate between good and bad bacteria, resulting in the destruction of all bacteria in your digestive tract. This will lead to a myriad of other problems as gut health is seen to be key to overall immunity and wellness.

luchschenF/shutterstock
To date, the FDA in the US does not collect data on the purpose of antibiotics drugs in animals, making it difficult to document the extent of the abuse of antibiotics in the agriculture sector. This is also true of many countries around the world. This is despite the fact that the C.D.C. estimates that more than 400,000 United States residents become ill with infections caused by antibiotic-resistant food-borne bacteria every year, with about one in five resistant infections caused by germs from food and animals. The C.D.C. says it is “working to prevent infections caused by this kind of bacteria,” through educating consumers and food workers about the prevention methods, whilst promoting the responsible use of antibiotics in both humans and animals.
The warning bells are no longer subtle idle warnings. Antibiotic resistance is a considered threat to positive health outcomes of not just this generation, but generations to come.
What can you do to protect yourself and your family?
1. Go grass-fed.
If you love your meat, then buy it smart. Farmer Angus explains that the best way to avoid developing antibiotic resistance is by ensuring you know where your meat comes from. In this quest, the word “grass-fed” is the one you’re looking for. Compared with feedlot meat, meat from grass-fed beef, bison, lamb, and goats has less total fat, saturated fat, cholesterol, and calories. Only use trusted grass-fed farmers and support your farming community to ensure a healthy supply. Poultry and even some farmed fish contain antibiotics, so the same circumspection applies.

Angus McIntosh, a biodynamic farmer based in Stellenbosch
2. Look for natural antibiotics.
“You can protect your body against infections and bacteria-based sickness by taking advantage of natural antibiotics and remedies that are available in the average kitchen,” says Robyn Smith, founder of the natural organic online store Faithful to Nature. Click here to find out more about which ones are the best in this quest.
3. Not antibiotics, but probiotics.
Ensure the health of your gut by taking care of the gut’s natural biome. Inside lives a plethora of healthy bacterial flora, which is estimated to make up about 70-85% of our immune system. Eat foods that bring good probiotics into your diet.
4. Strengthen your immune system
In the winter, most of us are bound to pick up a cold or two; this is normal. It can be prevented, by including foods rich in Vitamin C, such as kiwis, oranges, and grapefruits. Rest, avoid foods that are hard to digest, and cut out sugar. Manage your stress levels, sleep and importantly take regular exercise.
5. Eat less meat and poultry and increase vegetables, good fiber, and wild fish in your diet.
Studies over the years have shown that healthier diets include more fresh vegetables, good fiber, and wild fish. The longest living populations on Earth all enjoy diets with high intakes of vibrant veggies, no sugar, low dairy, and no wheat. So eat healthier stuff for better gut health and longevity.
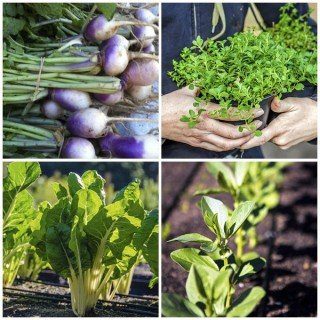
Image credit: Oranjezicht City Farm
6. Support bio-dynamic and organic farmers
And farmers who do not use antibiotics. Buy meat from farmers who produce grass-fed meat certified hormone and antibiotic-free. This is true of both beef, pork, and importantly poultry.
7. Take responsibility for your health
Make informed choices. Read the labels and understand what has been added to all your food, beverages, and supplements.
8. Don’t abuse or overuse pharmacological aids
They are there to help only when you really need it. Antibiotic resistance after all is a man (and woman) cause problems. It is our problem, which we can fix with the will to be healthier.
Written by Johané van den Berg and Gisèle Wertheim Aymés



![women [longevity live]](https://longevitylive.com/wp-content/uploads/2020/01/photo-of-women-walking-down-the-street-1116984-100x100.jpg)