More than 126 million U.S. adults reported experiencing chronic pain in the previous three months, according to a 2015 study in the Journal of Pain — 25.3 million contend with it every day, and 23.4 million say that it’s severe. If you’re one of those folks, you know that takes a huge toll, because persistent pain sets up a cycle of stress, frustration, limited mobility and decreasing overall healthfulness. The price tag for all this suffering? From $560 to $635 billion in 2010 dollars.
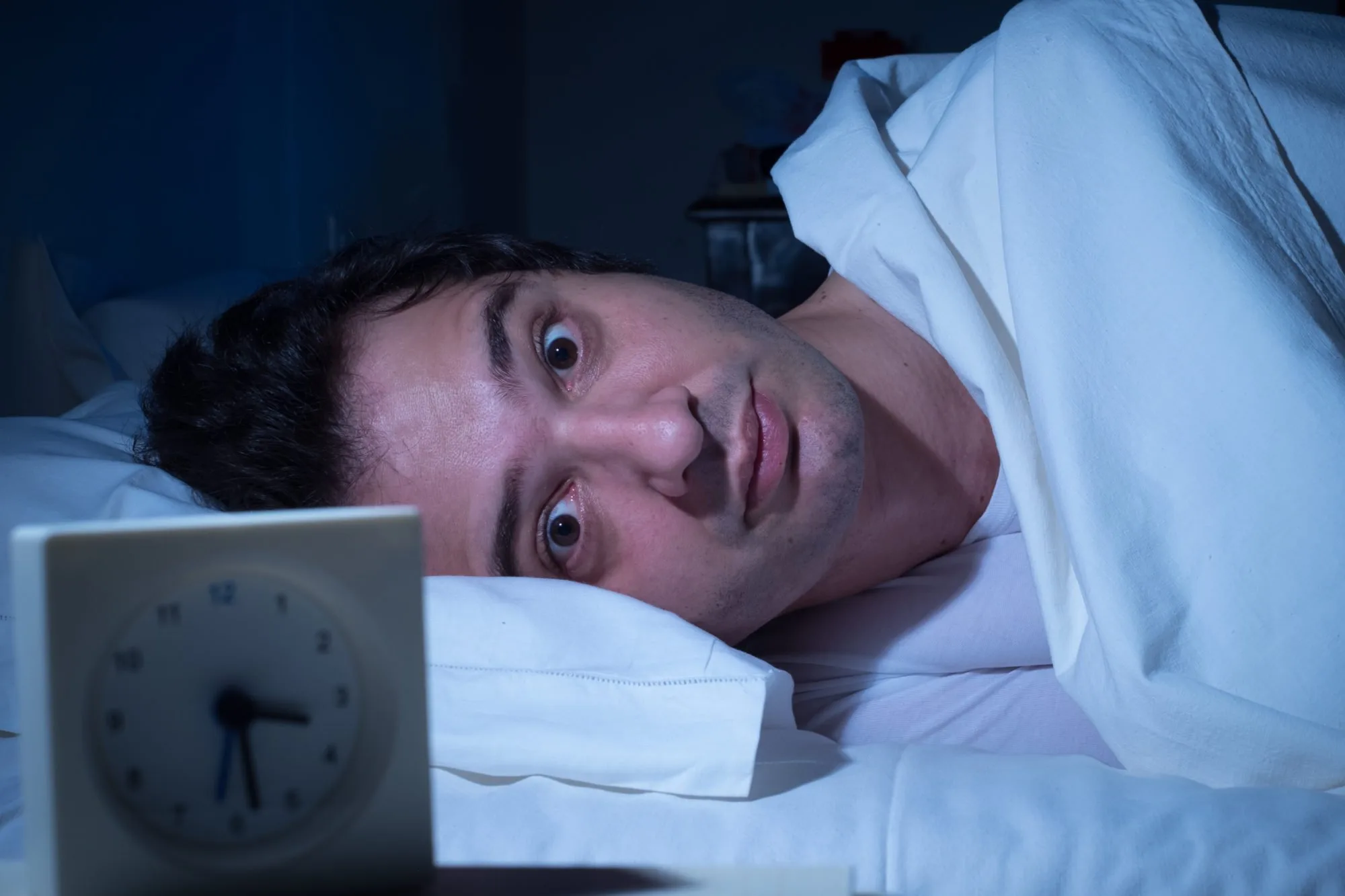
The Insomnia-Pain-Stress Cycle
A new study in the Journal of Clinical Sleep Medicine looked at the close relationship of insomnia and stress about pain to the anticipation and perception of pain and overall disruption of daily life. It revealed that attitudes toward pain and your response to the emotional and physical stress that’s triggered by pain interferes big time with sleep. One problem fuels the other, since lack of sleep increases inflammation.
That may be why folks with insomnia report twice as many days with spontaneous pain as those who don’t have sleep woes. And according to Dr. Mike’s Cleveland Clinic, 66 percent of people with chronic pain contend with insomnia, which increases their experience and/or intensity of pain.
What’s Hurting You?
 The most common causes of acute, recurring or chronic pain include abdominal pain, arthritis, back pain, fibromyalgia, gout, jaw pain, joint pain or stiffness, lupus, muscle or bone pain, neck pain, poor circulation in legs, recurring headache, rheumatoid arthritis, sprain or strain, severe headache or migraine and more. And whether you have young kids, are working or retired, you’ve gotta tamp down that pain to get a good night’s rest and get on with the business of daily life!
The most common causes of acute, recurring or chronic pain include abdominal pain, arthritis, back pain, fibromyalgia, gout, jaw pain, joint pain or stiffness, lupus, muscle or bone pain, neck pain, poor circulation in legs, recurring headache, rheumatoid arthritis, sprain or strain, severe headache or migraine and more. And whether you have young kids, are working or retired, you’ve gotta tamp down that pain to get a good night’s rest and get on with the business of daily life!
That’s one reason why, in any given week, some 23 percent of U.S. adults report using acetaminophen-containing products; 17 percent take aspirin or ibuprofen; 3.5 percent take naproxen; and in 2012 health-care providers wrote 259 million prescriptions for opioid pain medication — a 7.3 percent per capita increase since 2007. Unfortunately, at the same time, complications from use of those pain relievers soared too.
According to the Arthritis, Rheumatism and Aging Medical Information System and Consumer Reports, gastrointestinal bleeds and upset from NSAIDs are sending around 100,000 folks a year to the hospital. What’s more, 8 to 12 percent of people taking opioid medications for chronic pain become addicted. Clearly, even if taking pain relievers means less pain, it’s hardly a painless choice!
Breaking the Insomnia-Stress-Chronic-Pain Cycle
So what’s the first step you can take to improve your sleep, reduce your stress response to pain and ease the pain itself?
1. Recognize that sleep, stress and pain are interrelated.
 2. Take steps to reduce your anxiety about experiencing pain and your worry about how it interferes with your activities. Mindful meditation is very effective at dispelling the body’s physiological triggers of pain (cortisol and adrenalin) and keeping your mind from getting them all cranked up again. Also recommended: progressive muscle relaxation and guided imagery. (You might even try sleeping naked).
2. Take steps to reduce your anxiety about experiencing pain and your worry about how it interferes with your activities. Mindful meditation is very effective at dispelling the body’s physiological triggers of pain (cortisol and adrenalin) and keeping your mind from getting them all cranked up again. Also recommended: progressive muscle relaxation and guided imagery. (You might even try sleeping naked).
3. Physical activity (believe it) can help dispel stress and improve mobility, which can, in turn, ease pain. Chairbased or aquatic exercises can be effective if it’s difficult to move around on solid ground.
4. A healthy diet can diminish inflammation associated with pain. Say no to the Five Food Felons — added sugars or sugar syrups, trans and saturated fats and all processed grains; they all cause inflammation.
5. Cognitive-behavioral therapy can teach you new ways of thinking about sleep, pain and your relationship to both. Dr. Mike’s Cleveland Clinic website states that: “Through CBT work, there is an increased awareness of thoughts related to sleep, and once controlled, they tend to decrease and it is easier to fall asleep.”
Bottom line? Sleep disturbance due to pain is not an innocent event; try to manage the stress, but seek help from a professional if you can’t soothe the pain and increase your sleep within three weeks.
Here’s what you need to know before you reach for Melatonin to help you sleep.


![women [longevity live]](https://longevitylive.com/wp-content/uploads/2020/01/photo-of-women-walking-down-the-street-1116984-100x100.jpg)