We are what we eat – if there’s one thing you need to understand about nutrition and food allergies, it’s this. In this day and age, we face a big increase in negative ecological conditions. These include global warming, air, water, and soil pollution, climate change and other problems. As a result, we can expect that human bodies might face a large variety of functional and structural modifications. Also, the condition of the air, soil, water, and food products all influence the reactions. Especially since they take place within the living organisms. Finally, the reactions actively influence their functions, development, and even the duration of the organisms’ lives.
We encounter food allergies most commonly.
These actively impact not only people’s eating habits and approach to daily nutrition but also their overall quality of life. Now, one’s food preferences might cause the onset of some seriously disturbing symptoms or even death. However, it has become clear that food allergies are a major public concern that needs to be addressed appropriately and urgently. So, if we are what we eat, we have gone wrong somewhere.
How common are food allergies?
Is it really so widespread that we need to review not only our eating habits but our lifestyles as a whole? The latest studies have shown that the prevalence of food allergies is rapidly increasing. It is estimated to be detected in up to 10-% of the population (and particularly children) in developed countries[1]. However, there is still a lack of quality evidence regarding the actual prevalence of food allergies in different geographical regions. This is due to a large variety of reasons. Poor development of health care, for one, as well as the absence of electronic health records used for statistical purposes, and especially insufficient diagnoses of the condition.
Up to 15 million Americans have various allergic reactions to food.
Roughly two children in every classroom are likely to experience some sort of food allergy symptoms[2]. At the same time, researchers have shown that food allergy occurrence in China and Africa are rising at rates comparable to Western countries[1]. Interesting data arose from the research conducted by Loh and Tang 2018. It shows that in the context of the childhood population of different countries, the UK presents 4% of children suffering from food allergies. Denmark presented 3,6%, while Norway was at 6,8%. In Australia, this statistic was up to 4% in children of the age of 4[1].
Currently, there is a lack of conducted research in African countries. As a result, it is complicated to assess the situation with the prevalence of food allergies on the continent. However, scientists and physicians are now actively practicing the introduction of oral food sensitization challenges. These practices foresee the introduction of a specific food in small doses, which are slowly increasing by the physician to check the presence or development of an allergic reaction to certain foods. With this approach researchers have managed to detect that the prevalence of food allergies in African countries is very similar to developed countries[3]. The same study has shown that the sensitization rates to different foods in South India are 26.5%, which is also higher than in many countries of Europe or North America[3].
So what are food allergies?
A food allergy is an unusual or abnormal body reaction to a food sort. This is triggered by the body’s immune system. It can manifest in various symptoms. Sometimes the body can even develop certain conditions, which people are not always capable to recognize and address quickly. This makes a food allergy a medical condition, resulting in an abnormal immune response known as an allergic reaction. This reaction initially occurs because the human immune system begins to attack proteins in foods that would otherwise be harmless.
We find food allergies in both adults and children. The reasons for the cause and occurrence are still being investigated and actively debated.
The severity of a food allergy also varies from mild to potentially deadly.
Symptoms of food allergies include:
- Itching or swelling in the mouth
- Nausea, vomiting, diarrhea, abdominal pain and cramps
- Eczema or hives
- Tightening of the throat and difficulties in breathing (both inhaling and exhaling)
- Rapid blood pressure drop
The main major allergens are considered to be the following:
- Milk and milk-based products
- Eggs
- Fish (cod, bass, flounder)
- Crustacean shellfish (lobster, crab, shrimp)
- Peanuts
- Tree nuts (almonds, walnuts)
- Wheat
- Soybeans

Almost everyone has experienced at least one mild symptom of an unspecified allergic reaction. Whether it was boosted/triggered/caused by a food product, pollen, feather, animal fur, insulation, etc. Scientists still cannot fully explain this.
So you don’t really have to worry. It’s not just you, it happens to almost everyone. Not a big deal, right? Only unless it is.
Anaphylaxis
Anaphylaxis (anaphylactic shock) is a severe allergic reaction, which onsets extremely quickly and its symptoms can often be fatal. The most common causative agents of anaphylaxis are peanuts and other nuts, medications, and stinging insects (namely, their venom). It is important to rapidly detect the first symptoms of anaphylaxis.
This might include the following reactions:
- Mouth – itching, swelling of the tongue and lips (angioedema)
- Nose – stuffy or runny nose, sneezing
- Skin – itching, redness, hives, swelling
- Throat – itching, tightness, swelling of the back of the throat and swallowing
- Chest – shortness of breath, wheezing, coughing, chest tightness or pain
- Heart – weak pulse, shock, passing out
- Gastrointestinal tract – nausea, vomiting, diarrhea, cramps
- Nervous system – dizziness, increased alertness, panic, fainting, etc.
NOTE: the onset of anaphylactic shock is extremely rapid. It requires immediate action from the surrounding public. Immediately expel the product, medication, or stinger causing the condition and call emergency services. Sometimes anaphylactic shock might resemble a panic attack. However, the symptoms of a severe allergic reaction come after the first minute of contact with the allergen. – Any biological agent that is potentially causing an allergic reaction.
Food Intolerance
There is a difference between food intolerance and food allergies. Food allergies are a condition when the human body produces a specific response to the proteins (animal or plant) that the person consumes. These reactions might be Immunoglobulin E mediated (Ig-E) or not closely linked to the production of immunoglobulins. Immunoglobulins are a type of antibodies. Our immune system produces these antibodies to protect our body from different kinds of foreign proteins – bacteria and viruses. Immunoglobulins E sare the antibodies that elevate in the blood serum when a person develops an allergic reaction [5].
When the human body experiences an allergic reaction (read: immune response), it might develop even into a chronic inflammation if not treated right away. This can eventually lead to more complex conditions.
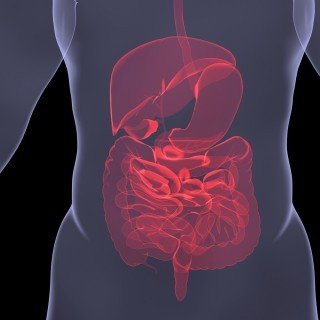
The digestive process
For example, when the main process of food digestion takes place in the intestines and the absorption in the bowel and the irritating proteins of the food are not eliminated or the condition is not treated, this might lead to gastroenteritis, colitis, autoimmune inflammation of the digestive tract and other intersected conditions [5,9].
On the contrary, food intolerance is something different. Unlike food allergies, if you suffer from food intolerance you suffer from the inability to completely digest a certain product or food. This can happen because the human body can’t produce essential enzymes for effective digestion of foods, the main processes that cause food intolerance to take place in the digestive system.
Examples of food intolerance:
1. Lactose intolerance
The body can’t digest lactose (a type of milk sugar) found in milk and many versions of dairy. It could have been inborn and acquired. Meaning that a person is born with lactase deficiency (an enzyme that breaks down lactose) or eventually acquired lactase deficiency. This can also occur when people consume fewer milk products or due to other medical reasons. (IBS, Crohn’s disease, pancreatic function deficiency, etc.). The main symptoms of lactose intolerance are bloating, gas, diarrhea, and even the alteration of the brush border membranes of the enterocytes of the small intestine. Brush border alterations can be dangerous when not properly diagnosed. Left untreated, it may eventually result in chronic enteritis (chronic inflammation of the small intestine) which can also manifest into IBS.
2. Gluten intolerance
In this case, the body can’t completely digest gluten. As you may know, this is a major plant protein found in rye, barley, and wheat. We need to think of gluten intolerance and celiac disease as two different conditions. In the case of gluten intolerance, people struggle with normal digestion of gluten. However, the body’s stress response to this protein does not include an autoimmune reaction. In the case of celiac disease, the trigger of a specific autoimmune condition is the consumption of gluten. This also causes inflammation in the lining of the small intestine, which eventually leads to nutrient malabsorption if not treated.
Celiac disease, however, onsets from early childhood. It might influence the normal development and growth of children. It can also cause anemia, skin rashes, abdominal bloating, and weight loss[10]. Celiac disease is also a genetically predisposed condition. While the reasons for gluten intolerance are not completely clear, it might also be linked to genetic protein defects[10, 12].
To summarize, usually, food intolerances are caused by:
- Absence of an enzyme required for food digestion
- IBS
- Sensitivity to food additives
- Recurring stress or mental health disorders
- Celiac disease
Chemical Sensitivity
Chemical sensitivity is an adverse reaction to chemicals found naturally or in consumed foods. People might often be sensitive to caffeine, food additives, preservatives, artificial flavors, chemicals with potential bioactivity such as amines, salicylates, glutamates and develop adverse reactions from asthma, urticaria and anaphylactoid responses to making their immune system more sensitive[17]. Active chemicals can also trigger such symptoms of the IBS as nausea, vomiting, diarrhea, abdominal pain, and bloating.
What Causes Food Allergies: The Microbiome Theory
It is widely known that four main allergic reactions occur within a specific pattern and onset[13]. However, while the reactions have already been studied, the main reasons why they occur in one person are and not that common in others still are under lively discussion. For example, if your parents have some sort of food or respiratory allergies, likely, you will also experience allergic symptoms at some point in your life. But there are other people whose parents also have allergies to various products or agents who are much more resistant to the development of allergic symptoms. Are they just lucky or is there more to it?
Well, scientists have recently been focusing on a relatively new and extremely fascinating concept – gut microbiota! The theory is that the composition of the good and sometimes not so good bacteria in your gut defines how allergic you can eventually become. Your gut’s microbiome is a whole ecosystem. This ecosystem is based on the mucous membrane of the human digestive system. It’s as influential and important as the human genes [4]. This astonishing finding was made possible because of the scientific curiosity of John Cryan, a neuroscientist, who was fascinated by the secrets of irritable bowel syndrome (IBS) and decided to take a deeper look into the gut.
A human’s gut microbiome is a boundless ecosystem
This ecosystem is composed of various microorganisms, from bacteria to fungi, that reside in the digestive tract (mainly in the colon). Up to 100 trillion bacteria reside there, which are responsible for breaking down toxins, food, producing vitamins and training the immune system.
Doctor Cryan and his colleagues decided to experiment on germ-free mice, initially investigating the linkage between gut microbiota and mental health. In their study, they managed to find that mice in the germ-free group experienced slow brain development and disorders in neuron contact[4]. Since then, other researchers have found connections between the condition of the gut microbiome and inflammation, allergies, functions of the immune system, appetite, digestive disorders, etc.
In the last decade, science has made an incredible advancement in the discovery of the gut microbiome as something unique and extremely individual. Years of research and observations managed to first discover that methods of delivering babies can cause their development of allergic reactions. We now know that C-section birth increases the risk of the development of allergic diseases in children [7].
These findings also caused scientists and physicians to find another connection.
This indicates that microbes are essential not only in establishing a properly functioning microbiome of the gut but also in maintaining healthy and adequate immune responses. At the first contact a child has with their mother, they embrace and communicate with the mom’s bacteria. This eventually becomes the baby’s first skin and digestive microbiome[7]. The more enriched and healthy the gut microbiome, the better for the children’s health and the lower the possibility of developing allergies in the future.
We can consider the development of autoimmune and inflammatory gut diseases, and even the onset of the initial symptoms of IBS under similar terms.
In short, the gut microbiome is still complicated and difficult to investigate. Much less to create a list of optimal compounds in the gut. However, it may be the next big thing for scientific and scholarly research to establish a comprehensive and healthy gut microbiome pattern. It is not only interlinked with allergy development but now there is now evidence showing a close possible connection with the possible onset of schizophrenia and bipolar disorder[6] – This is how important the microbiome is!
Can We Prevent Food Allergies?
The short answer is yes. But you have to start early and you have to do it intelligently. There are studies which found that children of women taking probiotics in their third trimester of pregnancy are less likely to develop food allergies [6]. Academics are still hesitant to recommend the ultimate probiotic. It’s an individual, just like one’s microbiome. Some studies have shown clinical results, but none of the scientific communities will recommend the usage of probiotics as an actual preventive measure. There is no “ideal probiotic” which is known to prevent the onset of the disease. For this reason, there is a need for further investigation of the changes in the gut microbe composition.
Another promising area of research is in an early allergen introduction. It sounds like a lot of fun, especially for the doctors, but not that much for parents. But actual evidential studies have shown that it works. Even more so for people who are genetically prone to developing allergic diseases. You need to start early with infants, which could also sound intimidating for parents. That’s why you should consult your pediatrician first before doing any food interventions to your newborn. From 2 to 8 months is the best period for the introduction of allergic products. It’s best to start with extremely small amounts and eventually increasing the quantity to reach an optimal tolerance dose. At this point, the person should not experience any symptoms of a food allergy[14].
IBS and Food Allergies
Some limited studies show a close interlink between IBS and food allergies. However, some scientists are still researching the possible connection between food allergies playing an important role in the development of IBS [11]. One study evaluated 122 people with IBS who also experienced different kinds of allergies. It has shown that these patients were more likely to have diarrhea as their main problem. The group of patients with no allergies was more prone to suffer from constipation as their main symptom of IBS.
Another study indicated that people with IBS experience more intensive symptoms of indigestion (diarrhea, constipation, cramps) after consuming specific foods[11]. After conducting allergic testing, it appeared that 60% of the examined patients had allergic reactions triggered by specific foods. IBS is one of the most widely-found gastrointestinal disorders in well-developed countries. However, it remains a partial mystery as therapeutic management of the condition is often unsatisfactory. On the other hand, foods do play a vital role in the onset of the symptoms of IBS. Also, most of the patients report observing a close connection between consumed foods and the severity of symptoms [17].
IBS patients also often develop secondary intolerance to different food items.
But it remains complicated to detect the mechanism of the development of the intolerance and symptoms induction. This is why modern scientists are actively supporting three main pathogenic mechanisms which can induce IBS symptoms:
- immune activation (hypersensitivity – allergy or autoimmune response)
- the direct action of food chemicals (bioactive molecules) and
- through luminal distention (lymph flow in the intestines)[17].
When looking closer at the theory of immune activation in the context of IBS, it could be considered that people with IBS can experience pathogenic reactions similar to those which people experience when having food allergies.






![women [longevity live]](https://longevitylive.com/wp-content/uploads/2020/01/photo-of-women-walking-down-the-street-1116984-100x100.jpg)










