PCOS – you’ve probably vaguely heard about it: something to do with ovaries and fertility. So what on earth is a dermatologist writing about it for?
Well, hormones and skin are a biggie and PCOS is one of the biggest culprits.
Considering that 1 in 10 women of childbearing age suffers from PCOS – the bigger question should be: why aren’t we talking MORE about it?
What is PCOS?
Polycystic ovarian syndrome is a cluster of symptoms ranging from the classical cysts on your ovaries to hormonal imbalances with an excess of androgens (male hormones), an out-of-whack female hormone profile to irregular or even absent menstrual cycles and obesity.
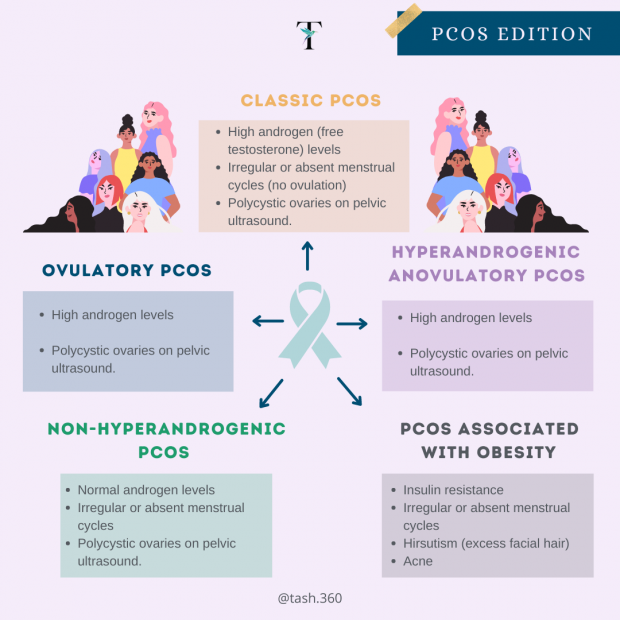
At med school, I was taught the ‘classical’ PCOS patient who would be obese with excess facial hair, severe acne and fertility issues. Today, we understand that there are many subtypes of PCOS, and women with PCOS may not even have cysts on their ovaries!
PCOS can be classified based on hormone profile, ovulation, and pelvic ultrasound findings:
4 Types of PCOS
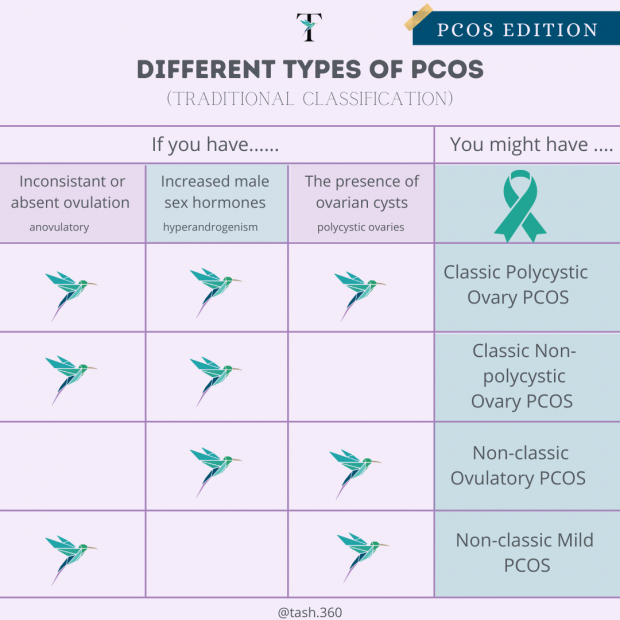
Different types of PCOS
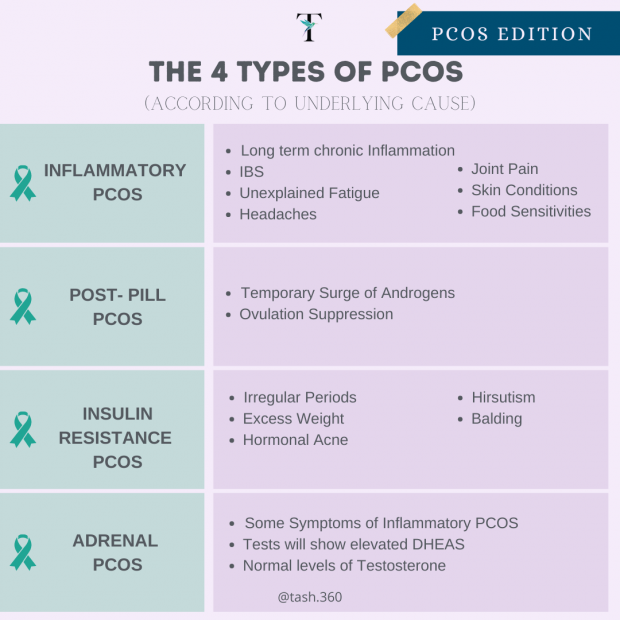
But more practical is categorizing PCOS according to underlying CAUSE which better guides treatment:
 So now let’s get back to how your skin may be waving a red flag that you have PCOS:
So now let’s get back to how your skin may be waving a red flag that you have PCOS:
There are 4 main skin signs of PCOS
•Adult female acne (AKA ‘hormonal’ acne): since androgens (for example testosterone or DHEAS) affect the hair follicles and increase sebum or oil production
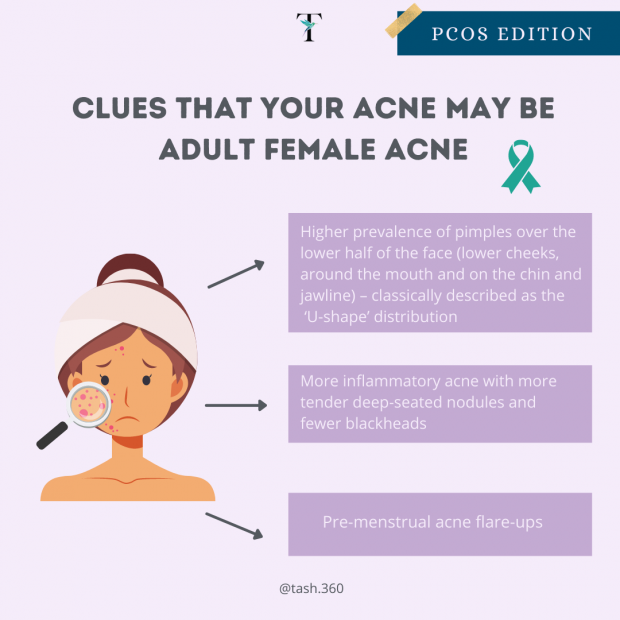
PCOS Clues
•Hirsutism: excessive hair growth in places where hair is usually absent or minimal for example on the chin, upper lip, neck, abdomen, around the nipples, chest, or back.
•Male pattern hair loss with thinning or balding of the hair on the crown of the head or with a receding hair line or diffuse hair loss. NOTE: This differs from a more female pattern of hair loss with widening of the hair path.
•Symptoms of insulin resistance such as acanthosis nigricans: dark, velvety areas of skin, usually in skin creases such as around the neck, groin and underarms or multiple skin tags (small skin growths) around your neck, under your breasts, groin or armpits.
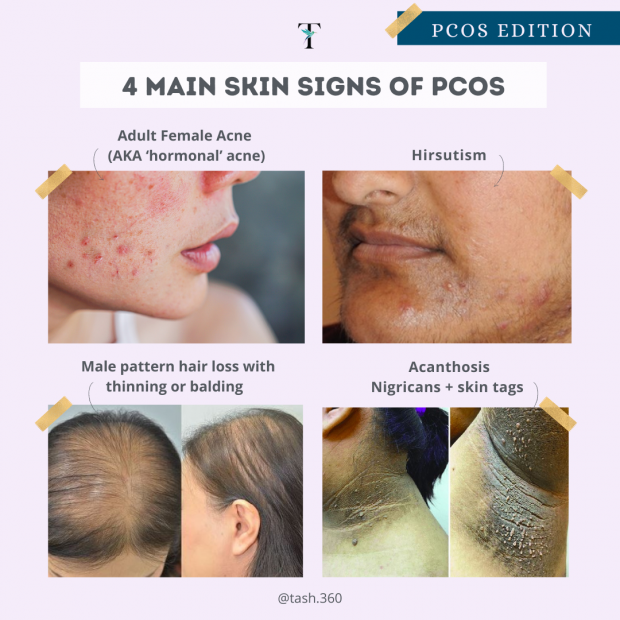
4 main Skin Signs of PCOS
I think that I fit this picture – now what?
The first step is to confirm the diagnosis through an in-depth history and clinical examination, together with blood work and a pelvic ultrasound.
Next comes treatment:
PCOS Treatment Options
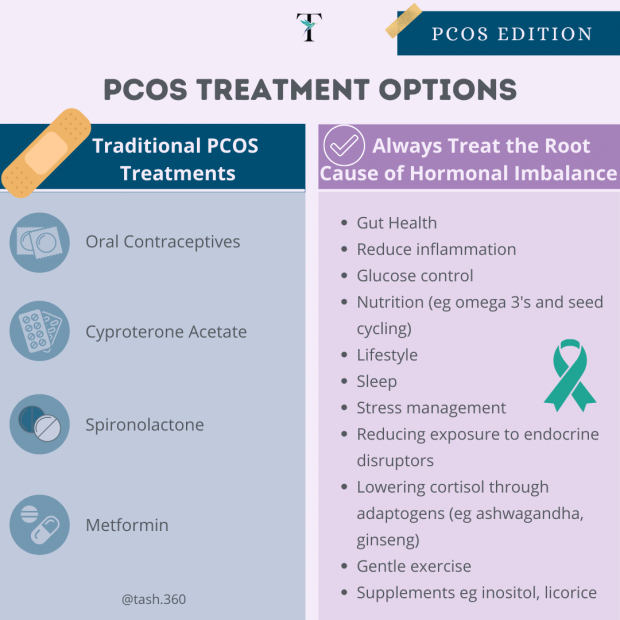
While traditional treatments focus on controlling symptoms with combined oral contraceptives or medications which block testosterone such as Androcur (cyproterone acetate) or spironolactone; treatments focusing on controlling insulin resistance (with traditional diabetes medications such as metformin) are also very effective.
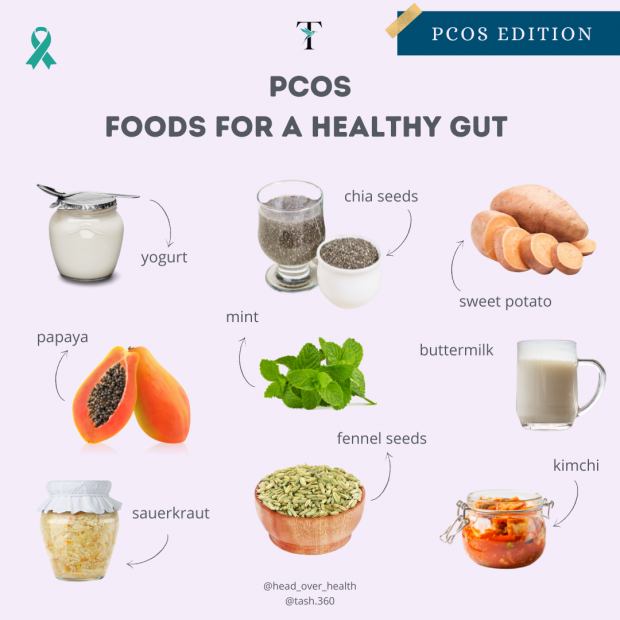
But stepping it back and looking at the ”root cause” when it comes to PCOS is critical and advanced hormone panels, glucose monitoring, and understanding your insulin sensitivity are key. Addressing inflammation, gut health and high stress levels through nutrition, lifestyle and stress management must ALWAYS play a role when it comes to addressing any hormonal imbalance.
PCOS FOOD
Look for multi-disciplinary teams which offer traditional ”quick-fixes” to manage symptoms while beginning the more involved ”long-haul” of correcting the underlying issues and releasing your skin from the shackles of PCOS.


![women [longevity live]](https://longevitylive.com/wp-content/uploads/2020/01/photo-of-women-walking-down-the-street-1116984-100x100.jpg)










